Do you always feel like you're standing on concrete pavement, even when you're wearing comfortable trainers? In the morning, do you get a sharp pain in your heels the moment your feet touch the ground? Do the soles of your feet ache terribly when you stand still? The thought of standing on hard surfaces make you cringe? Are you suffering with frequent injuries to your lower leg or ankle area?
If you answered yes to these questions, you might have a condition called plantar fasciitis. It affects an estimated 9.6% of middle-aged and older adults in the UK, and many younger people have it as well. The foot pain can quickly make living a normal life difficult.
Thankfully, there are plenty of plantar fasciitis treatments that can help reduce your symptoms. If you're ready to heal your heels, keep reading to learn more about the condition. What causes it, and what you can do to stop it.
What Is Plantar Fasciitis?
Your foot is full of bones, muscles, ligaments, tendons, and connective soft tissue called fascia. One large band of this connective tissue, known as the plantar fascia, runs across the bottom of your foot from your toes back to your heel.
Plantar fasciitis occurs when this band of connective tissue gets irritated and inflamed. Its most notable symptoms include:
- Sharp, searing, or stabbing pain in the heel and arch of the foot when weight-bearing
- Pain is most intense when getting out of bed in the morning or standing up after being sedentary
- Pain lessens as the day goes on
- Standing still for long periods or doing certain exercises worsens the pain
- Mild heel swelling
You might think a bit of heel pain is nothing to worry about, but plantar fasciitis can interrupt your life. Sometimes the pain is bad enough that you're unable to bear any weight on your foot. This can force you to take sick days from work, miss out on activities, and struggle to care for your family.
Some people feel this pain and believe they have heel bone spurs, small bone growths on the calcaneus (heel bone). While some people with plantar fasciitis do have heel spurs as well, they aren't often to blame for your symptoms. Heel spurs can be seen on X-rays ruling out other causes of heel pain, like a calcaneal stress fracture, arthritis or Baxter’s nerve entrapment.
Why Is Plantar Fasciitis Painful?
In reality, the reason plantar fasciitis hurts the way it does is due to tension.
If the arch of your foot is a hunting bow, the plantar fascia is the bowstring. This band of tissue works like a shock absorber, keeping the shape of your arch when you bear weight on your feet.
Laying down or sitting takes the pressure off the plantar fascia and relieves pain. As soon as you stand up, though—especially if you've let the bowstring get tight for a long time—that tension returns with a vengeance. Over time this can irritate the connective tissue and increase damage that leads to inflammation.
Most of us spend a lot of time on our feet every day. This means the inflammation never gets a chance to heal completely. It often gets worse, leading to chronic plantar fasciitis if left untreated.
Risk Factors and Causes for Plantar Fasciitis
Anyone can develop plantar fasciitis, but some people are at a higher risk for the condition than others.
According to NHS data, 60% of women and 67% of men in the UK fall into the categories of overweight or obese. Because carrying extra weight is a common cause of heel pain, it's no surprise that plantar heel pain is so familiar. This is even more of a concern for people with sudden weight gain, as their body isn't used to the stress.

Other factors that increase your chances of getting the condition include:
- Age (the condition often develops over age 40, though younger people can get it as well)
- Diabetes
- Arthritis
- Intense, high-impact activities like running
- A job that makes you stand or walk all day (teaching, manufacturing, healthcare, food service, etc.)
- Low or high arches, flat feet
- Overpronation (ankles roll inward when walking)
- Starting a new exercise programme
- General overuse and bad arch support footwear
Along with these concerns, even something as simple as wearing unsupportive shoes can irritate your plantar fascia.
Treatment of Plantar Fasciitis
The good news about plantar fasciitis is there are treatment options. If you have a mild case, you can take care of it at home. Otherwise, your GP and physiotherapist can help with your heel recovery.
Lowering Your Risk Factors
One of the best ways to promote foot recovery and health is to address any risk factors you can change.
If your job asks you to stand all day, swap out the high heels or fancy dress shoes for ones with good arch support, or shoe inserts (get custom orthotics—more on that later). If you're significantly overweight, dropping a few pounds can relieve a lot of the pressure on your feet. Patients that have diabetes or arthritis should be sure to manage those conditions carefully, as they can worsen plantar fascia inflammation.
You won't change every one of your risk factors, but even little adjustments can offer a lot of relief.
The RICE Method
When you need immediate relief from heel pain at home, try following the RICE method.
- Rest: sit down on a bed or sofa and stretch out your legs
- Ice: apply an ice pack to your heels in a cycle of 20 minutes on, 20 minutes off
- Compression: if your heels are swollen, you may want to wrap them with an elastic bandage or wear compression socks
- Elevation: rest your feet on cushioning and hold them above heart-level to reduce swelling
Following these steps won't cure your plantar fasciitis, but it can help with the symptoms. Try it after a long day of work or after going for a run.

Medications
Along with rest and ice, anti-inflammatory medicines like ibuprofen or over the counter, non-steroidal anti-inflammatory drugs can reduce your pain. Always ask your GP before taking any new medications. Also, follow the dosage instructions carefully—taking too many NSAIDs can lead to stomach, liver, and kidney problems.
Exercises and Stretches
Even though high-impact exercises can make heel pain worse, some types of activity namely, stretching exercises like gastrocnemius muscle stretches can improve it.
The easiest plantar fasciitis stretch involves standing in front of a wall. With your heel on the ground, lift your toes to touch the wall, straighten your leg, and step back with the other foot. Place your hands on the wall and gently lean forward to stretch your calf and achilles tendon muscles.
If you run or play sports, be sure to always warm-up and stretch out your calf muscles and heels before the activity. Make this part of your cool down routine as well.
You can also try massaging your feet to release tension. To do this, place a tennis ball on the ground, stand with your foot on top of it, and roll it back and forth under your arch while applying moderate pressure. If you want to combine stretching and icing, try using a frozen water bottle in place of a tennis ball.
Physiotherapy

If problems with your gait or misalignment are causing your heel pain, you might benefit from visiting a physical therapist. Physical therapy is a form of sports medicine and will help you get back to the game or sport you love, they will also help you from a recurrence of the injury.
A physiotherapist will analyse your gait for any abnormalities that put stress on your heels. Then, they'll help you strengthen weak areas to re-balance your stride. They may also give you a custom exercise and stretching program to do at home.
Your foot ankle specialist will also talk to you about extracorporeal shock wave therapy as a solution to helping with your recovery.
Custom Orthotics
Sometimes even the best shoes don't offer your feet the support they need. Other times, you have to wear unsupportive shoes due to dress codes. In either of these cases, custom orthotics can bring your feet back into alignment.
Custom orthotics are often 3D-printed, so they fit your foot's exact needs. They're durable, supportive, and can fit the inside of almost any closed boot or shoe.
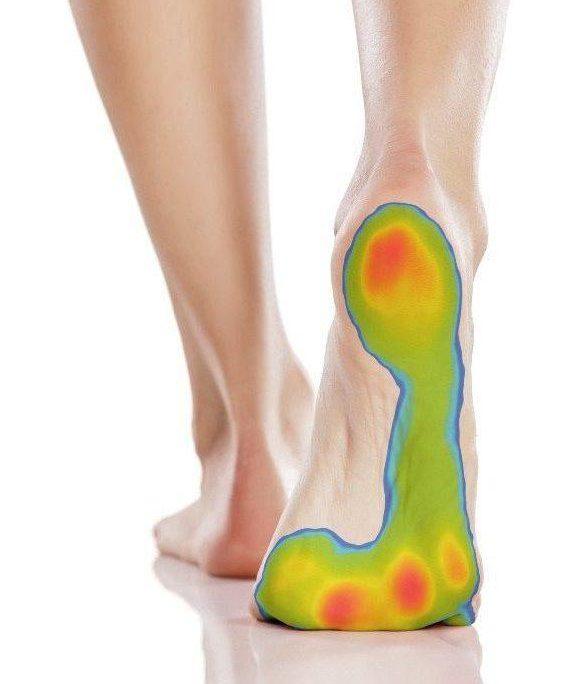
To get your plantar fasciitis insoles, you'll first have your gait assessed by a podiatrist. Podiatrists use the evidence-based dynamic foot-scanning technology to do a gait analysis along with manual measurements. The analysis creates a "pressure map" of where your feet bear the most weight.
Your podiatrist will use these results to design a pair of orthotics for you and send them off for printing. You can come back for a fitting in as little as two weeks. If your orthotics aren't right, your podiatrist will adjust them to the perfect fit while you wait.
Splints and Taping
In some cases, heel recovery requires a bit of extra support from splints or sports tape.
Wearing special plantar fasciitis splints at night can keep your connective tissue from tightening up while you sleep. The splint works by propping up your ankle and gently stretching out your calf.
Some people may find that they can't sleep while wearing a splint. If you're willing to wear it for a few hours before bed, it can still have a similar effect.
Otherwise, consider asking your physio to show you how to use sports tape. Unlike night splints, taping also offers support during the day. If you can't change your activity level to help your feet heal. It can prevent further injuries while decreasing your pain levels.
Pain-Relief Jabs
Another method of treating chronic inflammatory conditions like plantar fasciitis is with corticosteroid steroid injections. These pain-relief jabs, often full of cortisone or a similar medication, block pain receptors and reduce inflammation in the affected area.
The downside of steroid injections is that repeated doses can weaken the fascia. They may also cause more discomfort for the first few days after the injection and temporary numbness afterwards. As such, many orthopaedic doctors prefer to avoid them if possible.
Acupuncture and Chiropody
If you'd prefer to take the natural route, holistic medicines like acupuncture and chiropody are also effective plantar treatments.
Acupuncture works by stimulating your sensory nerves with carefully placed needles. While it may
sound painful, it actually causes your brain to release pain-relieving chemicals called endorphins. It can also reduce inflammation and promote faster healing.
One recent study investigated how well acupuncture worked as compared to cortisone jabs. They found steroid injections caused a rapid decrease in pain that either wore off or levelled out after three weeks. Dry needling acupuncture, in contrast, led to long-term pain reduction.
Surgical Procedures
If you've tried home remedies, conservative treatment or the plantar treatments on this list and nothing helps, your physio may recommend plantar fasciitis surgery. Candidates for this operation will have had pain that:
- Persists for six months or longer despite other remedies
- Significantly interferes with their life
- Is not the result of any other medical condition
If you're approved for the operation, your orthopaedic surgeon will make a small incision in the plantar fascia near the heel that releases the built-up tension. This procedure can either be a traditional open surgery or an endoscopic operation. Either way, you'll likely to be able to go home the same day.
Healing from plantar fasciitis surgery depends on which type of operation you have. Endoscopic surgery is less invasive, so you may be able to walk within a few days. If you have open surgery, you might have to wear a protective boot cast for a few weeks.
You'll have to be gentle and avoid activities like running or jumping for the next few months. Because your foot's support system is weaker after the surgery, it's also even more important that you wear supportive shoes.
Talk to Your Medical Provider About Plantar Fasciitis Treatments Today
No one should have to live with constant, debilitating pain. If you're suffering, don't wait another day. Ask your medical provider about which plantar fasciitis treatments are right for you.
If you don't have a physiotherapist of your own, contact The Medical Healthcare Centres for medical advice. Our private healthcare locations are spread across the UK, so there's sure to be a branch near you. Feel free to phone us or book an online video consultation with one of our excellent GPs, physiotherapists, or chiropodists.
The Medical remains open
As a fully registered and regulated medical provider, we will remain OPEN during COVID. We are committed to providing consistent, uninterrupted medical care, whilst taking the necessary precautions to keep everyone safe. Click here for more information and to see what changes we've made to protect you.

